Spine Pain Patients Who See Chiropractors First Need Fewer Healthcare Services: Study
By Zachary Cupler, DC, Alyssa Troutner, DC, Clinton Daniels, DC Most chiropractors are very familiar with the fact that spine...
By Zachary Cupler, DC, Alyssa Troutner, DC, Clinton Daniels, DC Most chiropractors are very familiar with the fact that spine...
Earlier this year, ACA member Kenneth Weber, DC, PhD, was awarded two grants totaling more than $5 million from the...
Chiropractic integration into hospitals and other collaborative interdisciplinary environments remains aspirational for many recent graduates and seasoned providers alike; as...
Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review. (Ammendolia C, et al.1) Good science...
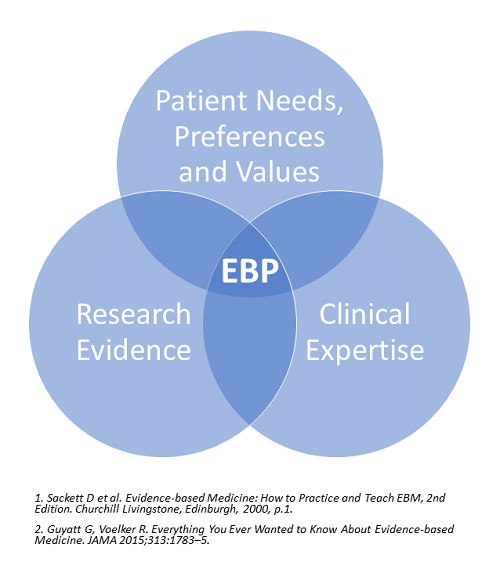
There is an abundance of definitions and variation of terms for evidence-based practice (EBP), including evidence-informed practice and evidence-based clinical practice (EBCP). Fortunately, most of them say essentially the same thing. The most well-known definition is that put forth by David Sackett and colleagues:
“Evidence-based [practice] is the integration of best research evidence with clinical expertise and patient values.”1
Evidence-based practice (EBP) is a term coined by Gordon Guyatt2 at McMaster University in 1991 to encompass the idea of teaching clinicians how to find, interpret and use the best available evidence for clinical practice. Evidence-based clinical practice (EBCP)–often used synonymously with EBP–is a patient-centered approach to clinical management that explicitly utilizes research evidence, patient values and clinician experience. The strength of that evidence, the benefits and risks of alternative approaches and patient preferences all influence management strategies.
With the focus on greatest patient benefit, ACA’s Evidence-Based Practice in Chiropractic Management policy (PDF) supports these principles as a means to incorporate current best evidence into all aspects of clinical care.
The American Chiropractic Association and Palmer College of Chiropractic partnered to provide the following series of articles and videos that translate how the findings of research studies and other evidence can be applied in clinical practice.
Sensitization (Part 1): Characteristics and Implications
By Anna-Marie Schmidt, MM, DC, and Robert Vining, DC, DHSc
Sensitization (Part 2): Management Strategies
By Anna-Marie Schmidt, MM, DC, and Robert Vining, DC, DHSc
“Chronic Pain: Screening for Potential Psychological Factors”
By Anna-Marie Schmidt, MM, DC, and Robert Vining, DC, DHSc
“Best Practice Recommendations: Translating Evidence Into Action”
By Anna-Marie Schmidt, MM, DC, and Robert Vining, DC, DHSc
“Social Factors: A Sometimes-overlooked Opportunity”
By Anna-Marie Schmidt, MM, DC, and Robert Vining, DC, DHSc
“Developing Person-centeredness: A Continual Process”
By Anna-Marie Schmidt, MM, DC, and Robert D. Vining, DC, DHSc
“Choosing Outcomes Assessments for Back Pain”
By Kara Shannon, DC, and Zacariah Shannon, DC, MS
“Improving Interprofessional Communication”
By Heather Mai-Roecker, DC, ARNP, and Christopher B. Roecker, DC, MS
“Collaboration for Low Back Pain Treatment in Older Adults”
By Zacariah Shannon, DC, MS
> Listen to the author discuss the article in this video.
“Does Spinal Manipulation Affect Central Nervous System Pain Mechanisms?”
By Zacariah Shannon, DC, MS, Robert Vining, DC, and Stephen Onifer, PhD
> Listen to the author(s) discuss the article in this video.
“Enhancing a Biopsychosocial Approach”
By Robert Vining, DC, and Yasmeen Khan, DC
“Interpreting ‘Quality’ and ‘Strength’ in a Practice Guideline”
By Robert Vining, DC, and Zacariah Shannon, DC, MS
“Relative Energy Deficiency in Sport (RED-S)”
By Robert Vining, DC, and Breanne Bovee, DC