By Anna-Marie Schmidt MM, DC, and Robert Vining, DC, DHSc
Chronic pain symptoms and the ability to manage and cope with them can be strongly influenced by what are generally referred to as psychological factors.1 These factors have the capacity to substantially hinder clinical improvement, cause symptom aggravation and reduce self-management capacity.1–4 Though these concepts are well-supported in the scientific literature, they are not inherently usable. Practical methods of revealing relevant psychological factors are needed.
To explore whether psychological factors are clinically relevant, clinicians can ask questions during the consultation and/or use one of several screening questionnaires. Asking individualized questions can be effective, though this strategy may be difficult to employ consistently. Using questionnaires as a standard procedure ensures screening occurs systematically. In this article, we address office-based questionnaires designed to screen for key psychological factors that can influence clinical outcomes.
An Illustration
Consider a person with chronic low back pain symptoms; no underlying pathology is present. In this example, we will assume this person receives appropriate diagnosis and treatment for the biological (physiological) aspects of their case. Nevertheless, this person experiences limited improvement.
What other information could be important to know about this person? Such a person may feel distressed or discouraged. They may have recently experienced an emotionally traumatic event. They may think symptoms will not improve or are destined to worsen over time. Physical activities (e.g., yard work, cycling) might be avoided or discontinued due to pain and/or concerns over worsening a condition. Each of these possibilities can potentially contribute to poor response or limited self-management capacity.
Several questionnaires can be used to screen for the types of negative factors described above.5 Because questionnaires involve varying amounts of time, effort and resources, some may not be feasible in all clinical settings. However, doing so can potentially save time when the process helps reveal negative psychological factors.
Questionnaires
Self-efficacy: Judgement of personal capacity to accomplish activities (mental, physical, lifestyle, etc.) that positively influence a condition.2
Dwelling on personal deficiencies, giving up quickly at a difficult task, being hesitant to try new exercises and/or lacking commitment to goals can be signs of low self-efficacy.6 Because low self-efficacy can adversely affect treatment adherence, lead to increased pain intensity, greater disability and reduced physical functioning, it is important to identify.3 Two validated questionnaires measuring self-efficacy are:5
- Pain Self-Efficacy Questionnaire (PSEQ): A 10-item questionnaire assessing confidence in performing activities despite experiencing pain.7,8
- 2-item version of the Pain Self-Efficacy Questionnaire (PSEQ-2): An abbreviated form of the PSEQ.7
Higher PSEQ scores indicate stronger self-efficacy beliefs. The PSEQ-2 is considered a robust measure of self-efficacy and suitable for clinical use.7 Because it consists of only two questions, it may be the easiest to implement in a busy practice setting.
Fear of movement: Fear of executing movement(s) or physical activity that is wrongfully assumed to cause reinjury.9
Aberrant movement strategies can develop out of need or from fear that certain positions or movements will cause pain or injury. Unnecessary fear of movement can lead to greater levels of pain intensity, pain severity, disability, and lower quality of life.4 Three validated questionnaires measuring fear of movement are:5
- Fear Avoidance Beliefs Questionnaire (FABQ): A 16-item patient-reported questionnaire assessing beliefs about how physical activity and work affect low back pain.10
- Tampa Scale for Kinesiophobia (TSK): A 17-item questionnaire measuring the subjective experience of kinesiophobia. It is also designed to discriminate between non-excessive fear and phobia among persons with chronic musculoskeletal pain.11,12
- 11-item version of the Tampa Scale for Kinesiophobia (TSK-11): A shortened form of the TSK offering the advantage of brevity and removal of all inversely scored items.13,14
Higher scores indicate stronger fear avoidance beliefs for all questionnaires.10,13
Practical Application
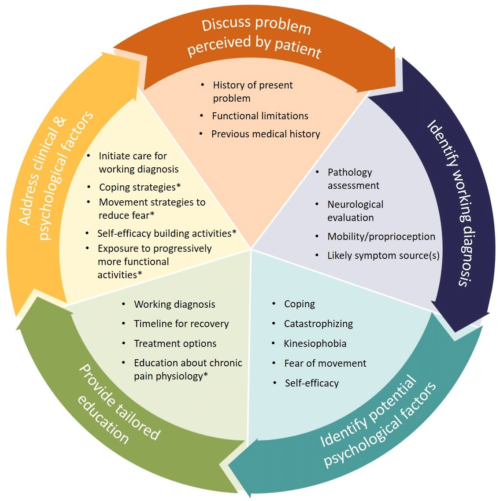
Using a questionnaire is a practical way to ensure screening is standardized across all patients. Responses provide evidence for or against the potential existence of impactful psychological factors that can be investigated further. Discussion generated by screening data can provide information to inform tailored education and other strategies focused on individual needs. Figure 1 (left) displays a proposed model for identifying and addressing psychological factors as part of a biopsychosocial clinical evaluation and management process. (*Utilize when applicable)
Identifying symptoms and biological (physiological) aspects of a condition occurs in the first two steps. The third step focuses on identifying potential psychological factors. While listed as the third step in the process, identifying psychological factors may occur at any point and outside of an initial visit.
Together the first three steps inform education and management strategies that address relevant biological and psychological factors. Though specific education and management strategies for psychological factors are beyond the scope of this article, the overall process is designed to include periodic re-evaluation, adapting education and management focus during each cycle as part of a whole-person approach to care. For some, identifying and addressing psychological factors can be the most important element for enabling clinical improvement.
Information resources for instruments designed to screen for or measure a variety of psychological factors may be found in the appendix following the reference section below.
Additional Questionnaires to Consider
Catastrophizing: A mental and emotional response to pain consisting of pain magnification, rumination, and feeling helpless to manage pain.2
- Pain Catastrophizing Scale (PCS): A patient-reported questionnaire consisting of 13 items assessing three distinct components of catastrophizing.20
- Coping Strategies Questionnaire (CSQ): A 48-item self-report questionnaire measuring the use of cognitive and behavioral strategies to cope with pain.21
Coping: The use of behavioral, emotional, and cognitive techniques to manage symptoms of distress.2
- Revised Coping Strategies Questionnaire (CSQ-R): A shortened version of the CSQ consisting of 27 patient-reported items.21
- Coping Strategies Questionnaire (CSQ): A 48-item self-report questionnaire measuring the use of cognitive and behavior strategies to cope with pain.21
- Chronic Pain Coping Inventory (CPCI): Questionnaire consisting of 65 items assessing 11 coping strategies.22
Anna-Marie Schmidt MM, DC, is a post-doctoral research scholar at the Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
Robert Vining, DC, DHSc, is associate dean of clinical research at the Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
References
- Edwards RR, Dworkin RH, Sullivan MD, Turk D, Wasan AD. The role of psychosocial processes in the development and maintenance of chronic pain disorders. J Pain. 2016;17(9 Suppl):T70-T92. doi:10.1016/j.jpain.2016.01.001
- Meints SM, Edwards RR. Evaluating psychosocial contributions to chronic pain outcomes. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2018;87:168-182. doi:10.1016/j.pnpbp.2018.01.017
- Martinez-Calderon J, Zamora-Campos C, Navarro-Ledesma S, Luque-Suarez A. The Role of Self-Efficacy on the Prognosis of Chronic Musculoskeletal Pain: A Systematic Review. The Journal of Pain. 2018;19(1):10-34. doi:10.1016/j.jpain.2017.08.008
- Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J Sports Med. 2019;53(9):554-559. doi:10.1136/bjsports-2017-098673
- Sleijser-Koehorst MLS, Bijker L, Cuijpers P, Scholten-Peeters GGM, Coppieters MW. Preferred self-administered questionnaires to assess fear of movement, coping, self-efficacy, and catastrophizing in patients with musculoskeletal pain-A modified Delphi study. Pain. 2019;160(3):600-606. doi:10.1097/j.pain.0000000000001441
- Picha K, Howell D. A model to increase rehabilitation adherence to home exercise programmes in patients with varying levels of self-efficacy. Musculoskeletal Care. 2018;16(1):233-237.
- Nicholas MK, McGuire BE, Asghari A. A 2-Item Short Form of the Pain Self-Efficacy Questionnaire: Development and Psychometric Evaluation of PSEQ-2. J Pain. 2015;16(2):153-163.
- Nicholas MK. The pain self‐efficacy questionnaire: Taking pain into account. Eur J Pain. 2007;11(2):153-163.
- Martinez-Calderon J, Flores-Cortes M, Morales-Asencio JM, Luque-Suarez A. Pain-Related Fear, Pain Intensity and Function in Individuals With Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. The Journal of Pain. May 2019. doi:10.1016/j.jpain.2019.04.009
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157-168.
- Hudes K. The Tampa Scale of Kinesiophobia and neck pain, disability and range of motion: a narrative review of the literature. J Can Chiropr Assoc. 2011;55(3):222-232.
- Lundberg MKE, Styf J, Carlsson SG. A psychometric evaluation of the Tampa Scale for Kinesiophobia – from a physiotherapeutic perspective. Physiother Theory Pract. 2004;20:121-133.
- Woby S, Roach N, Urmston M, Watson P. Psychometric properties of the TSK-11: A shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117(1-2):137-144.
- Larsson C, Hansson E, Sundquist K, Jakobsson U. Psychometric properties of the Tampa Scale of Kinesiophobia (TSK-11) among older people with chronic pain. Physiother Theory Pract. 2014;30(6):421-428.
- Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. March 2019:bjsports-2018-099878. doi:10.1136/bjsports-2018-099878
- Murphy D, Jacob G, Seaman D, Steven H. Clinical Reasoning in Spine Pain. Volume 1 Primary Management of Low Back Disorders Using the CRISP Protocols. Vol 1. Pawtucket, RI: CRISP Education and Research, LLC; 2013.
- Watson JA, Ryan CG, Cooper L, et al. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. The Journal of Pain. March 2019. doi:10.1016/j.jpain.2019.02.011
- Bunzli S, Smith A, Schütze R, Lin I, O’Sullivan P. Making Sense of Low Back Pain and Pain-Related Fear. J Orthop Sports Phys Ther. 2017;47(9):628-636. doi:10.2519/jospt.2017.7434
- Booth J, Moseley GL, Schiltenwolf M, Cashin A, Davies M, Hübscher M. Exercise for chronic musculoskeletal pain: A biopsychosocial approach. Musculoskeletal Care. 2017;15(4):413-421. doi:10.1002/msc.1191
- Sullivan MJL. The Pain Catastrophizing Scale. User manual. http://sullivan-painresearch.mcgill.ca/pdf/pcs/PCSManual_English.pdf.
- Hastie B, Riley J 3rd, Fillingim R. Ethnic differences in pain coping: factor structure of the coping strategies questionnaire and coping strategies questionnaire-revised. J Pain. 2004;5(6):304-316.
- Tan G, Nguyen Q, Anderson K, Jensen M, Thornby J. Further validation of the chronic pain coping inventory. J Pain. 2005;6(1):29-40.
Appendix
Instrument Question Sources
| Instrument | Source Publication |
| Pain Self-Efficacy Questionnaire (PSEQ) | Nicholas MK. The pain self‐efficacy questionnaire: Taking pain into account. Eur J Pain. 2007;11(2):153-163. |
| 2-item version of the Pain Self-Efficacy Questionnaire (PSEQ-2) | Nicholas MK, McGuire BE, Asghari A. A 2-Item Short Form of the Pain Self-Efficacy Questionnaire: Development and Psychometric Evaluation of PSEQ-2. J Pain. 2015;16(2):153-163. |
| Fear Avoidance Beliefs Questionnaire (FABQ) | Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157-168. |
| Tampa Scale for Kinesiophobia (TSK) | Lundberg MKE, Styf J, Carlsson SG. A psychometric evaluation of the Tampa Scale for Kinesiophobia – from a physiotherapeutic perspective. 2004;20:121-133. |
| 11-item version of the Tampa Scale for Kinesiophobia (TSK-11) | Larsson C, Hansson E, Sundquist K, Jakobsson U. Psychometric properties of the Tampa Scale of Kinesiophobia (TSK-11) among older people with chronic pain. Physiother Theory Pract. 2014;30(6):421-428. |
