ABSTRACT
Objective: The purpose of this case report is to demonstrate the positive outcome of utilizing flexion distraction and decompression spinal manipulation for the treatment of adjacent segment disease related to a C5-C6 block vertebra (Klippel-Feil Disease).
Clinical Features: A 71-year-old male presented with chronic recurring neck pain and stiffness. His symptoms were worsened by his leisure activities and limited his activities of daily living. His cervical spine x-rays revealed a non-segmentation anomaly at C5-C6 with adjacent segment disease.
Intervention and Outcome: This patient was treated solely with flexion distraction and decompression manipulation performed to the cervical spine. His treatment encompassed 16 visits over 16 weeks, and he made significant progress regarding the severity and frequency of his pain and his ability to perform his activities of daily living.
Conclusion: This case demonstrates the positive outcome for the treatment of cervical adjacent segment disease resulting from a non-segmentation anomaly utilizing flexion distraction and decompression manipulation.
CLINICAL PRESENTATION
A 71-year-old male presented with complaints of recurring intermittent neck pain and stiffness over the past five years. He describes the pain as a constant nagging ache in his neck that can get severe and radiate to his right upper back and shoulder. The pain limits his activities of daily living at times. An increase in pain is usually precipitated by excessive activities such as golf and yard work. This episode occurred after a three-day golf trip. His numerical pain scale (NPS) (0 no pain – 10 worst pain scale) indicated the pain varies from 2 to 8 with an average pain level of 5. His neck disability index (NDI) was rated at 36%. He denied any radiation of pain past the shoulder and denied any numbness or upper extremity weakness.
Prior interventions included oral methylprednisolone (Medrol dose pack), which provided minimal temporary relief. He also underwent 14 sessions of physical therapy and was given posture exercises to perform at home. The patient reported no decrease in the frequency or severity of his symptoms from these interventions.
EXAMINATION
His cervical range of motion examination revealed flexion at 50 degrees causing a pulling sensation, extension 30 degrees causing pain in his neck and upper back on the right, right and left lateral flexion were 15 and 25 degrees respectively, right rotation was 55 degrees with pain and left rotation was 60 degrees. Palpation revealed tenderness and a decrease in inter-segmental motion at multiple cervical levels. His upper extremity sensation and strength were normal bilaterally and reflexes diminished globally. Hypertonicity to palpation was noted at the suboccipital, trapezius I and II, levator scapulae, rhomboids and splenius capitus muscles. Anterior head carriage, rounded shoulders and tight pectoralis muscles were noted.
AP and lateral plain film cervical spine radiographs were performed. Sagittal plane alignment demonstrated an anterior head carriage with loss of lordosis. Intervertebral disc space was decreased at C3-C4, C4-C5 and C6-C7. A non-segmentation anomaly was noted at C5-C6 involving the anterior and posterior arches. Uncinate proliferation was noted at C5 and C7 and facet arthrosis at C2-C3. See Figures 1 and 2.
IMAGING

Figure 1
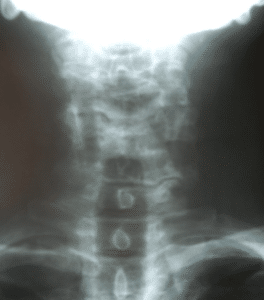
Figure 2
TREATMENT INTERVENTION
Treatment consisted solely of flexion distraction and decompression (FDD) spinal manipulation to the cervical spine. Prior to treatment, tolerance testing was performed. Tolerance testing involves gentle long-y axis distraction of each spinal segment starting at the atlanto-occipital level, then the C1 spinous process proceeding inferiorly at each spinal level to the C7 level. Careful distraction testing at the C7 level avoids any posterior to anterior pressure on C7 spinous process, which research shows may increase intradiscal pressures. 1 A rare event, lateralization of pain is monitored, which would indicate a different approach for the visit such as acupressure, ice, trigger point therapy, or gentle massage.
Following the algorithms of decision-making for FDD protocols for cervical spine and due to the lack of any radicular component to the patient’s subjective and objective findings, FDD Protocol 2 was used. 18 Protocol 2 allows for range of motion adjusting – lateral flexion, rotation, flexion, extension, and coupled motion – of each cervical spine segment as long-y axis distraction is applied so that the spinal canal is opened during motion application.
Treatment for FDD started with 10 repetitions of axial decompression contacting the occiput, followed by axial decompression and rotation at the clinically indicated spinal levels at C3-C4, C4-C5 and C6-C7. After the first two treatments, coupled movements of axial decompression, rotation, and lateral flexion were added with axial decompression first then each motion with it.

Figure 3 – Protocol 2
The schedule of care included two visits a week for two weeks followed by one visit a week for 10 weeks, then two additional visits at two week intervals seeking 50% of pain relief, which would indicate a shift in treatment protocol (1 to 2 if radiculopathy is present) as well as visit frequency (reduced by 50%). After the 16th visit over a period of 16 weeks, the patient was released from active care. During the course of care, this patient reported a progressive decrease in the severity and frequency of his symptoms. He continued to report an increase in complaints after prolonged golf and yard work; however, these flare-ups were noticeably less severe and of less duration. This patient reported a great deal of satisfaction with his ability to perform the activities he enjoys more frequently and for a greater duration without having significant increases in his pain and stiffness.
At the time of his release from active care, his numerical pain scale (NPS) indicated his pain ranged from 0 to 4 with an average of 2. His neck disability index (NDI) was rated at 12%. The cervical range of motion examination revealed an increase globally when compared to the initial findings, however, still with some limitations.
DISCUSSION
A rare skeletal disorder predominantly characterized by abnormal union or fusion of two or more bones of the spinal column (vertebrae) within the neck (cervical vertebrae), Klippel-Feil Syndrome (KFS) (congenital cervical vertebral fusion) is reported to affect some KFS individuals with an abnormally short neck, restricted movement of the head and neck, and a low hairline at the back of the head (posterior hairline). Present at birth (congenital), KFS may be undiagnosed if it is mild until later in life when symptoms worsen or first become apparent. For some, KFS can be associated with a variety of additional symptoms and physical abnormalities like abnormal curvature of the spine (scoliosis) and/or vertebral instability, spina bifida occulta, raised scapula (Sprengel’s deformity), absent rib(s) and other rib defects including cervical ribs, other skeletal abnormalities including skeletal malformations of the ear, nose, mouth and larynx including hearing impairment and cleft palate, malformations of the head and facial (craniofacial) area; anomalies of the urinary tract and/or kidney including absent or horse-shoe kidney; or structural abnormalities of the heart (congenital heart defects), mirror movements, webbing of the digits and digital hypoplasia. Further, neurological complications for some KFS individuals are reported due to associated spinal cord injury. KFS may be inherited as an autosomal dominant or autosomal recessive trait. Researchers have determined that some cases of KFS are associated with mutations of the GDF6 gene on chromosome 8.2 Only a small number of patients with KFS and congenital scoliosis are reported to develop cervical symptoms with fusion of the cervicothoracic junction and congenital cervical stenosis being factors that lead to a greater incidence of cervical symptoms. 3
Klippel and Feil were the first to describe this syndrome most completely in 1912. The typical KFS disorder is reported to result from a failure of the normal segmentation of the somites during weeks 3–8 of gestation. Feil reported in 1919 additional cases and distinguished between three morphologic groups. The incidence of KFS has been estimated to be approximately 1:40,000–42,000 births with a slight female predilection (≥ 65%) noted. Children with fused cervical vertebrae, with or without craniocervical anomalies, are reported to be at risk of injury to the upper cervical cord and medulla from relatively minor trauma. 4
Seventy percent of KFS patients have been reported to have scoliosis. Three types of KFS are described with single level fusions being most common. 4
- Type I: displays a massive fusion of many cervical and upper thoracic vertebra with synostosis
- Type II: the fusion is at only one or two interspaces with hemivertebrae, occipitoatlantoid fusion and other abnormalities in the cervical spine
- Type III: shows cervical fusions associated with lower thoracic or lumbar fusion
The literature has reported on many related conditions occurring with KFS. Respiratory failure was reported in a 28-year-old woman diagnosed with KFS who had a deformed thorax and kyphoscoliosis.5 Sacral agenesis, low lying cord, lipomyelomeningocele and split cord malformation presenting with tethered cord syndrome have been reported with KFS. 6 A surgical series of patients with cervical spine myelopathy revealed a high prevalence of KFS possibly indicating that these patients are disposed to increased biomechanical use of segments adjacent to fused vertebra. The tendency of patients with KFS to present with more extensive MRI evidence of degeneration than non-KFS patients with cervical spine myelopathy supported this hypothesis. 7 Tourette syndrome and Klippel Feil anomaly in a child with chromosome 22q11 duplication is documented. 8 Patients with KFS are particularly susceptible to cervical cord injury after a minor fall or a major traumatic episode. An unusual case of KFS where the patient had disc prolapse between two Klippel-Feil segments is presented, and the difficulties in the management of the case is described. 9 Agenesis of the right carotid artery associated with KFS is reported. 10 One series of 20 KFS cases reported one of the highest rates of ear involvement in KFS showing that 12 (60%) displayed most of the reported ear abnormalities such as microtia, external ear canal stenosis, chronic ear inflammations and their sequels, anomalies of the tympanic cavity and ossicles, inner ear dysplasia, deformed internal acoustic canal, and wide vestibular aqueduct. No correlation between the identified ear pathologies and the skeletal and extraskeletal malformations was discovered. The genetic nature of the syndrome was supported by the existence of affected family members in 4 (20%) of the cases. 11
Neuroimaging of a patient who experienced recurrent and transient episodes of quadriplegia which imitated cervical cord neurapraxia showed congenital intersegmental fusion of C5 through C7 (consistent with Klippel-Feil anomaly) as well as corresponding abnormal spinal cord signals on T2-weighted images and enhancing focal lesion opposite the C4 vertebral body. The episodic quadriplegia has not recurred after a posterior cervical decompression at C4-C5 and lateral mass fixation was done. 12 Cervical ribs are seen more frequently in Klippel-Feil anomaly. 13 X-ray images and CT scans of a 61-year-old woman with extremity numbness, sensory impairment, muscular weakness, and tendon hyper-reflexia revealed assimilation of the atlas to the occipital bone, C2 and C3 fusion, abnormal passage of the vertebral arteries, and an anomalous bony mass on the right lateral mass of the atlas protruding into the spinal column. 14
FDD spinal manipulation is documented to relieve conditions with pain related to the cervical spine as well as Klippel Feil Syndrome. Diagnosed with C2-C3 block vertebrae with occipitalization of atlas and degenerated discs, a 34-year-old female with severe neck, shoulder, arm pain of months’ duration found relief of symptoms with flexion-distraction manipulation in 8 treatments over 2 months. 15 FDD is reported to relieve pain due to cervical disk herniation, foraminal narrowing, and associated radiating pain and radiculopathy in the left upper extremity of a patient in 10 visits over 4 weeks. 16 A retrospective study of 39 cases of cervical radiculopathy treated with cervical flexion distraction spinal manipulation revealed a statistically significant reduction in pain measured by visual analog scale scores in a mean of 13.2 visits. 17
The Klippel-Feil Syndrome is seen in chiropractic practice, and its accompanying neurological and musculoskeletal manifestations must be considered. Familiarity with treatment options as presented in this case may well benefit chiropractic patients.
CONCLUSION
This is a case of a 71 year-old man with chronic recurring symptoms related to a cervical block vertebrae, Klippel-Feil Disease, and adjacent segment degenerative changes and joint dysfunction. He responded well to FDD spinal manipulation for cervical spine utilizing Protocol 2. Reasonable expectations were discussed with this patient regarding the degree of resolution of his subjective and objective findings. He was pleased that his progress decreased the severity and frequency of his symptoms and allowed a return to his daily and leisure activities
REFERENCES
- Gudavalli M, Potluri T, Carandang G, et al. Intradiscal Pressure Changes during Manual Cervical Distraction: A Cadaveric Study. Evidence-Based Complementary and Alternative Medicine, 2013; Article ID 954134, 10 pages, doi:10.1155/2013/954134. https://www.hindawi.com/journals/ecam/2013/954134/
- Klippel Feil Syndrome, NORD National Organization for Rare Disorders, accessed on September 16, 2017, https://rarediseases.org/rare-diseases/klippel-feil-syndrome/
- Theiss SM, Smith MD, Winter RB. The Long-Term Follow-Up Of Patients With Klippel-Feil Syndrome And Congenital Scoliosis. Spine, 1997; 22(11): 1219-1222. https://www.ncbi.nlm.nih.gov/pubmed/9201859
- Thomsen MN, Schneider U, Weber M, Johannison R, Niethard JR. Scoliosis And Congenital Anomalies Associated With Klippel-Feil Syndrome Types I-III. Spine, 1997; 22(4): 396-401. https://www.ncbi.nlm.nih.gov/pubmed/9055366
- Suga K, Motoyama K, Hara A, Kume N, Matsunaga N, Kametani P, Matsuzaki M. Respiratory Failure And Pulmonary Hypertension Associated With Klippel Feil Syndrome. Annals of Nuclear Medicine, 1999; 13(6): 441-446. https://www.ncbi.nlm.nih.gov/pubmed/10656282
- Satyarthee GD, Kumar A. Klippel-Feil Syndrome Associated with Sacral Agenesis, Low Lying Cord, Lipomyelomeningocele and Split Cord Malformation Presenting with Tethered Cord Syndrome: Pentads Neural Tube Defects Spread along Whole Spinal Axis. J Pediatr Neurosci, 2017; 12(1): 51-54. doi: 10.4103/1817-1745.205651. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5437790/
- Nouri A, Tetreault L, Zamorano JJ, Mohanty CB, Fehlings MG. Prevalence of Klippel-Feil Syndrome in a Surgical Series of Patients with Cervical Spondylotic Myelopathy: Analysis of the Prospective, Multicenter AOSpine North America Study. Global Spine J, 2015; 5(4): 294-9. doi: 10.1055/s-0035-1546817. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4516751/
- Clarke RA, Fang ZM, Diwan AD, Gilbert DL. Tourette Syndrome And Klippel-Feil Anomaly In A Child With Chromosome 22q11 Duplication. Case Rep Med, 2009; 361518. doi: 10.1155/2009/361518. https://www.hindawi.com/journals/crim/2009/361518/
- Agrawal A, Badve AM, Swarnkar N, Sarda K. Disc Prolapse And Cord Contusion In A Case Of Klippel-Feil Syndrome Following Minor Trauma. Indian J Orthop, 2009; 43(2): 210-2. doi: 10.4103/0019-5413.50857. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2762260/
- Braga M, Pederzoli M, Beretta S, Ferrarini M, Canovaro P, Arpaia G, Crespi V. Agenesis Of The Right Internal Carotid Artery And Klippel-Feil Syndrome: Case Report. Spine (Phila Pa 1976), 2009; 34(20): E740-2. doi: 10.1097/BRS.0b013e3181b41181. https://www.ncbi.nlm.nih.gov/pubmed/19752694
- Yildirim N, Arslanoğlu A, Mahiroğullari M, Sahan M, Ozkan H. Klippel-Feil syndrome and associated ear anomalies. Am J Otolaryngol, 2008; 29(5): 319-25. doi: 10.1016/j.amjoto.2007.09.009. https://www.ncbi.nlm.nih.gov/pubmed/18722888
- Gupta SN, Piatt JH Jr, Belay B. Cervical Spinal Cord Neurapraxia In The Setting Of Klippel-Feil Anomaly: A Diagnostic And Therapeutic Challenge. Spinal Cord, 2007; 45(9): 637-40. https://www.ncbi.nlm.nih.gov/pubmed/17130888
- Tubbs RS, Salter EG, Oakes WJ. Klippel-Feil Anomaly With Associated Rudimentary Cervical Ribs In A Human Skeleton: Case Report And Review Of The Literature. Folia Morphol (Warsz), 2006; 65(1): 92-4. https://www.ncbi.nlm.nih.gov/pubmed/16783749
- Kagawa M, Jinnai T, Matsumoto Y, Kawai N, Kunishio K, Tamiya T, Nagao S. Chiari I Malformation Accompanied By Assimilation Of The Atlas, Klippel-Feil Syndrome, And Syringomyelia: Case Report. Surg Neurol, 2006; 65(5): 497-502; discussion 502. https://www.ncbi.nlm.nih.gov/pubmed/16630916
- Kruse RA, Schliesser J, DeBono VF. Klippel-Feil Syndrome With Radiculopathy. Chiropractic Management Utilizing Flexion-Distraction Technique: A Case Report. J of Neuromuscular System, 2000; 8(4): 124-131. https://www.researchgate.net/publication/291767516_Klippel-Feil_Syndrome_with_Radiculopathy_Chiropractic_Management_Utilizing_Flexion-Distraction_Technique_A_Case_Report
- Manison AM. Chiropractic management using Cox cervical flexion-distraction technique for a disk herniation with left foraminal narrowing in a 64-year-old man. Journal of Chiropractic Medicine, 2011; 10(4): 316-321. doi:10.1016/j.jcm.2011.04.004. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3315856/
- Schliesser J, Kruse R, Debono V. Cervical radiculopathy treated with chiropractic flexion distraction manipulation: a retrospective study in a private practice setting. Journal of Manipulative & Physiological Therapeutics, 2003; 26(9): 592-596. http://www.jmptonline.org/article/S0161-4754(03)00154-4/abstract
- Cox JM: Neck, Shoulder and Arm Pain: Mechanism, Diagnosis, Treatment. 4th Fort Wayne IN: Cox Technic Resource Center, Inc., 2014; 105-106.
AUTHORS
Ralph Kruse, DC, FACO
A 1990 graduate of National University of Health Sciences, Dr. Ralph Kruse has earned certification in Cox® Technic, diplomate status with the American Board of Chiropractic Orthopedics, and fellow status with the Academy of Chiropractic Orthopedists. He has authored numerous peer-reviewed papers, participated in flexion distraction studies as clinician/researcher at National, Palmer, and Loyola Stritch School of Medicine, and taught lumbar and cervical Cox® Technic certification courses and state association presentations around the world. He maintains private practices in Chicago and Homewood.
http://www.coxchirocare.com/
James M. Cox, DC, DACBR, FACO(H)
A 1963 graduate of National College of Chiropractic, Dr. Cox enjoys a long professional life in chiropractic. He is the developer of Cox® Technic flexion distraction; author, Low Back Pain (7th), Neck, Shoulder, and Arm Pain (4th), peer-reviewed articles; editorial board member, JMPT; co-researcher/clinician, biomechanical/clinical studies with National, Palmer, Loyola Stritch School of Medicine; diplomate, American Chiropractic Board of Radiology; presenter, spine conferences. He practices in Fort Wayne, Indiana, and consults with fellow physicians via Fort Wayne Chiropractic Radiological Center.
