Chiropractic: A Cost-Efficient Option for Medicare Patients

Practicing chiropractors offer their patients a broad-based approach to pain management, including manual manipulation of the spine and extremities, joint mobilization, soft-tissue massage techniques, physiological therapies, exercise instruction and activity advice. This safe, non-pharmaceutical approach has been proven to be a highly effective option for many patients with musculoskeletal pain1,2, and the evidence is clear that adding currently covered services performed by doctors of chiropractic for patients in Medicare will not add additional costs to the program.
Unfortunately, Medicare currently only reimburses for a single chiropractic service: manual manipulation of spine-related conditions. This artificial barrier limits chiropractors’ ability to provide their patients with the full range of effective treatments included in their legal scope of practice and educational training. It also burdens Medicare patients with significant financial hardships by limiting their freedom of choice in health care – a burden not affecting patients of other providers. Additionally, Medicare does not reimburse chiropractors for performing the Evaluation and Management services necessary to establish the safety of manipulation and to formulate the most effective treatment plan for patients — even though CMS policy and professional standards of care require doctors of chiropractic to provide these essential services.
The following is a synopsis of evidence demonstrating the clinical and cost-effectiveness of chiropractic management for various common musculoskeletal conditions:
Chiropractic Use Decreases Costs for Medicare Patients with Low Back Pain
One recent study found that older multiple-comorbid patients who used only chiropractic manipulative therapy (CMT) during their chronic low back pain episodes had lower overall costs of care, shorter episodes and a lower cost of care per episode day than patients in the other treatment groups. Further, costs of care for the episode and per episode day were lower for patients who used a combination of CMT and conventional medical care compared with patients who did not use CMT.3
Chronic Low Back Pain
According to a report by the U.S. Agency for Healthcare Research and Quality, spinal manipulation, exercise, acupuncture and psychological therapies all produced gains in short-term function compared with usual (medical) care or inactive controls. Effects on intermediate-term function and pain were sustained for spinal manipulation, psychological therapies and multidisciplinary rehabilitation.4
Another article in the Journal of Family Practice endorsed a select group of therapies that show “good-quality patient-oriented evidence” for managing chronic low back pain, and the authors recommend “a trial of either acupuncture or spinal manipulation for patients with chronic LBP.”5
Neck Pain
A large study of the North Carolina State Employees’ Health Insurance Plan found that chiropractic care, alone or when combined with medical (MD) care, incurred appreciably fewer costs for patients with either complicated or uncomplicated neck pain.6
Headache
Another study of the North Carolina State Employees’ Health Insurance Plan found MD care and chiropractic (DC) care, alone or in combination, were the least expensive patterns of headache care. Risk-adjusted charges were significantly less for DC-only care.7
Extremity Conditions
A comprehensive review in 2010 found evidence for the effectiveness of manual treatment (including manipulation, mobilization and massage) for numerous common extremity conditions, including shoulder pain, tennis elbow, hip and knee osteoarthritis, plantar fasciitis and fibromyalgia.8 Currently, Medicare does not cover chiropractic treatment for extremity conditions.
Chiropractic Care Decreases Opioid Use
Another important consideration is the additional indirect costs incurred by patients using (and often abusing) opioid drugs. Opioids are now the most commonly prescribed class of drugs for the treatment of back pain, despite very limited evidence of their safety and long-term effectiveness. More than half of regular opioid users report back pain.9 One recent study found that patients who received services from a doctor of chiropractic for back pain were significantly less likely to fill a prescription for an opioid medication than other patients.10 Another study found that the likelihood of an adverse drug event occurring in an outpatient setting within 12 months was 51% lower among recipients of chiropractic services as compared with nonrecipients.11
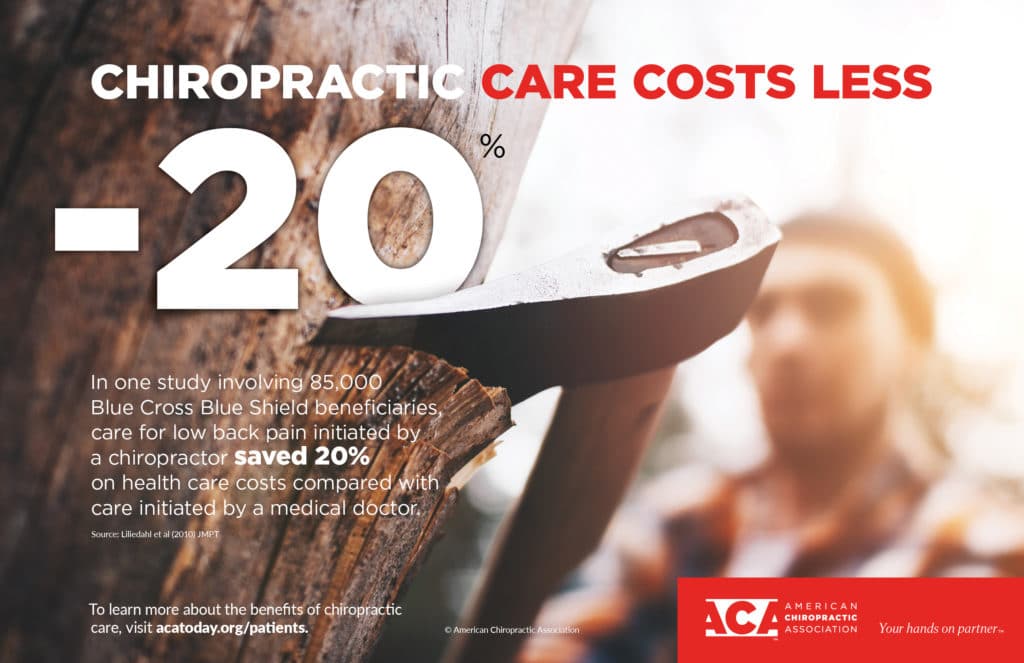
The American Board of Family Medicine published a recent study showing that, “For Medicare patients with back and/or neck pain, availability of chiropractic care reduces the number of primary care physician visits, resulting in an annual savings of $83.5 million.”12 An analysis of Optum claims revealed that “Healthcare plans that formally incorporate chiropractic typically realize a 2:1 return for every dollar spent.”13 A similar study by BC/BS of Tennessee found that “Low back pain care initiated with a doctor of chiropractic (DC) saves 40 percent on health care costs when compared with care initiated through a medical doctor (MD).”14
Multiple federal policymakers, including the Food and Drug Administration, the Centers for Disease Control and Prevention, the Department of Defense, and the Joint Commission (which accredits all major healthcare systems in the United States) have endorsed non-pharmacologic therapies including chiropractic as a first-line treatment for pain.15-19
Conclusion
Coverage of the full range of services a Medicare patient can receive by a doctor of chiropractic under most commercial insurance products will likely result in lower costs. This will happen due to decreased use of expensive diagnostic tests, over-prescribed pharmaceuticals, such as opioids, and unnecessary referrals to specialists.
Approving the proposed legislative changes to Medicare will remove artificial barriers that prevent Medicare patients from benefiting from the full range of safe, clinically effective treatments offered by doctors of chiropractic, and allow patients to access this widely recommended and cost-efficient care.
References:
1. Nonpharmacologic treatment of chronic pain: What works? J Family Pract 2018 67:8 (Aug) 474-83.
2. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166(7):514-530. doi: 10.7326/M16-2367
3. The association between use of chiropractic care and costs of care among older Medicare patients with chronic low back pain and multiple comorbidities. J Manipulative Physiol Ther. 2016 (Feb); 39(2): 63–75.e2. doi:10.1016/j.jmpt.2016.01.006
4. The US Agency for Healthcare Research and Quality recently published a systematic review of more than 218 publications regarding the effectiveness of various non-pharmacologic treatments for chronic pain. Noninvasive Nonpharmacological Treatment. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Jun. Report No.: 18-EHC013-EF. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0099929/
5. Nonpharmacologic treatment of chronic pain: What works? J Fam Pract. 2018 Aug;67(8):474;477;480;483.
6. Variations in Patterns of Utilization and Charges for the care of Neck Pain in North Carolina, 2000 to 2009: A Statewide Claims’ Data Analysis. J Manipulative Physiol Ther 2016;39:240-251. doi: 10.1016/j.jmpt.2016.02.007
7. Variations in Patterns of Utilization and Charges for the care of Headache in North Carolina, 2000 to 2009: A Statewide Claims’ Data Analysis. J Manipulative Physiol Ther 2016;39:229-239. doi: 10.1016/j.jmpt.2016.02.008.
8. Effectiveness of manual therapies: the UK evidence report. Chiropractic & Osteopathy 2010, 18:3 http://www.chiroandosteo.com/content/18/1/3
9. Opioids for Low Back Pain. BMJ 2015;350:g6380. doi: https://doi.org/10.1136/bmj.g6380
10. Association Between Utilization of Chiropractic Services for Treatment of Low-Back Pain and Use of Prescription Opioids. J Altern Complement Med. 2018 Jun;24(6):552-556. doi: 10.1089/acm.2017.0131. Epub 2018 Feb 22.
11. Association Between Utilization of Chiropractic Services for Treatment of Low Back Pain and Risk of Adverse Drug Events. J Manipulative Physiol Ther. 2018 Jun;41(5):383-388. doi: 10.1016/j.jmpt.2018.01.004. Epub 2018 May 26.
12. Davis MA, et al. Regional Supply of Chiropractic Care and Visits to Primary Care Physicians for Back and Neck Pain. Journal of the American Board of Family Medicine: JABFM. 2015;28(4):481-490.
13. Feldman V, Return on investment analysis of Optum offerings — assumes Network/UM/Claims services; Optum Book of Business Analytics 2013. Analysis as of 12/8/2014.
14. Liliedahl RL, Finch MD, Axene DV, Goertz CM. Cost of care for common back pain conditions initiated with a chiropractic doctor vs medical doctor/ doctor of osteopathy as first line physician: experience of one Tennessee-based general health insurer. J Manipulative Physiol Ther. 2010;33:640–643.
15. Green BN, et al. Integration of Chiropractic Services in Military and Veteran Health Care Facilities: A Systematic Review of the Literature. Journal of Evidence-Based Complementary & Alternative Medicine. 2016 Apr;21(2):115-30.
16. FDA Education Blueprint for Health Care Providers Involved in the Management or Support of Patients with Pain. May 2017. Accessed on May 12, 2017.
17. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49.
18. The Official Newsletter of The Joint Commission. Joint Commission Enhances Pain Assessment and Management Requirements for Accredited Hospitals. July 2017 Volume 37 Number 7. Ahead of print in 2018 Comprehensive Accreditation Manual for Hospitals.
19. Joint Commission Online. Revision to Pain Management Standards. http://www.jointcommission.org/assets/1/23/jconline_november_12_14.pdf
