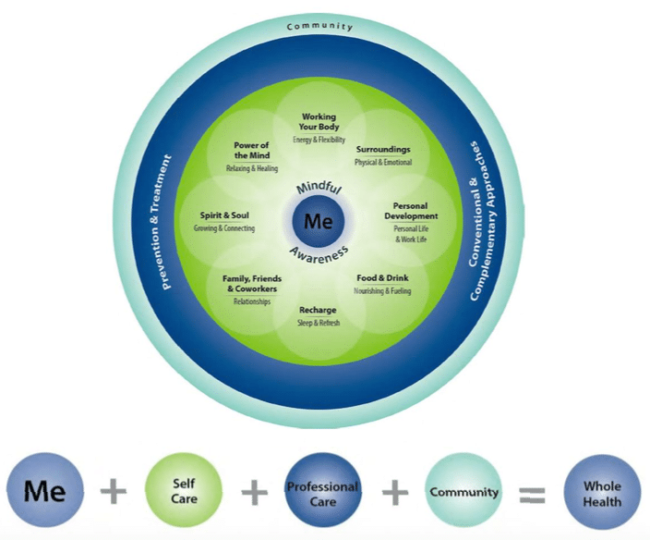
Starting this year, the Department of Veterans Affairs (VA) is launching its Whole Health System in each of the 18 Veterans Integrative Service Networks (VISN). This will be done via one flagship site in each VISN to assist veterans through self-empowerment, self-care, and clinical treatment. As part of my residency, I’ve been introduced to the program and have attended an orientation.
The process of whole health can begin at any point the veteran chooses, though typically it’s initiated when they seek to establish care within VA. First, they will be connected with a health coach who will sit down and discuss what the patient desires with regard to his specific needs. Subsequently, the veteran will fill out a patient health inventory, a tool that’s designed to get to the heart of what matters most to them. Questions are designed to determine what brings them joy, where they rate themselves with regard to physical, mental and emotional well-being, how they’re sleeping, what their current diet consists of, the strength of their relationships and coping abilities. This is an excellent jumping off point to get the veteran started along their path to health and wellness.1
The self-empowerment segment will be carried out through the Pathway portion of the program where veterans are encouraged to explore their personal goals and aspirations for care. Example goals could be to reduce pain, improve function or have a better quality of life. The veteran might say, “I want to play with my grandkids”, “I’d like to play a whole round of golf”, or “I wish I could improve my sleep”. Obviously, each veteran is different and his or her personal goals will vary, which is why the first component of the program is important and the self-empowerment aspect will be the starting point for the veteran to figure out what means the most.
The second component, self-care, is accomplished via well-being programs that focus on equipping the veteran with tools to support personal goals. Through self-care and parts of complementary and integrative health such as yoga, tai chi, and mindfulness, the veteran will be equipped to better manage his pain. He might also learn breathing techniques, stretches, home exercises or stress-reduction skills.
The last component of the program incorporates providers who will utilize a whole health approach, including complementary and integrative care such as chiropractic and acupuncture. This is where we as chiropractors come into the picture and have an opportunity to provide pain management services and lifestyle modifications to promote a better quality of life for the veteran. These options for care will be available at VA or in their community.2
With regard to pain management on a broader level, active treatments (aspects the patient does for himself or herself) should be at the forefront of any quality healthcare plan. This could include modifying posture, performing corrective exercise, exercising regularly in the community, meditating on a regular basis or performing good sleep hygiene. Passive treatments (things the patient has done for or to them) should serve as an adjunct.3 These aspects of care include chiropractic, acupuncture, soft tissue manipulation, electrical muscle stimulation, therapeutic ultrasound and low-level laser therapy. Research suggests that active treatments for chronic low back pain are typically effective.4
Overall, the whole health program was designed to empower, equip and treat out nation’s veterans to provide better outcomes and improved quality of life. This approach to treatment is revolutionary in its approach due to the collaborative nature and holistic overview. It’s my understanding that VA hopes this model will become the future standard of care in America and I’m optimistic this dream will someday soon become a reality.
Dr. Huybrecht is the chiropractic resident at the VA St. Louis Healthcare System under program director Pamela Wakefield, DC. He is working toward completion of the Certified Chiropractic Sports Physician program and certification in chiropractic acupuncture. Dr. Huybrecht’s professional interests include chronic pain management for veterans, organizational leadership, and state and national advocacy.
Whole Health Care Management Resources5
- Chiropractic
- Acupuncture
- Animal-assisted therapy
- Art therapy
- Biofeedback
- Chronic disease self-management
- Counseling
- Diabetes prevention
- Health Coaches
- Health Partner Support
- Massage
- Meditation
- Mindfulness based stress reduction
- Movement therapy
- Music therapy
- Physical activity
- Tai Chi
- Therapeutic journaling
- Tobacco cessation
- Weight management (MOVE program)
- Yoga
Whole Health Circle6
References
- Whole Health Personal Health Inventory https://www.va.gov/PATIENTCENTEREDCARE/docs/Personal-Health-Inventory-final-508-WHFL.pdf
- Expanding VA Whole Health System https://www.va.gov/PATIENTCENTEREDCARE/features/Expanding_the_VA_Whole_Health_System.asp
- Loranger L. Good practice: active vs. passive treatments. Physiotherapy Alberta News. https://www.physiotherapyalberta.ca/physiotherapists/news/good_practice_active_vs._passive_treatments?page=12
- Mannion A, Muntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24:2435–2448. [PubMed]
- Whole Health Program Guide PDF, https://www.va.gov/PATIENTCENTEREDCARE/docs/2017-AR-Vet-Facing_FNL-W508.pdf
- Whole Health Circle, http://projects.hsl.wisc.edu/SERVICE/veteran-materials/new/WHItStartsWithMe_508.pdf
